Parenting
The parenting blog resource for The Healthy Mummy. What to expect and how to prepare for your new baby. Plus parenting advice you will actually use for kids of all ages. Expert advice and information for teething babies, as well as behavioural advice for tweens. The online mothers support group for The Healthy Mummy.

100 baby names with POWERFUL meanings
What's in a name? Well, a whole lot if you look at these 100 baby boy and girl names. Name meanings may make you like that name even more! Choosing the perfect name for your baby can be a challenge. If you're looking for strong baby names with meaning we've compiled a list of powerful baby names that are sure to inspire and empower your little one. Check out our post below!

Expert Tips To Stop Money Problems Ruining Your Relationship
Money can’t buy you love, but it can cause many problems for couples. In fact, it’s one of the…

9 Reasons Why Mothers Should ALWAYS Trust Their Instincts
You’ve given birth to your beautiful baby, you’ve signed the discharge papers and you bundle your babe up in a…

14 cute baby names inspired by EASTER
Some parents go down the route of naming their children after festive things like Christmas - but apparently there’s a heap of Easter names out there too!

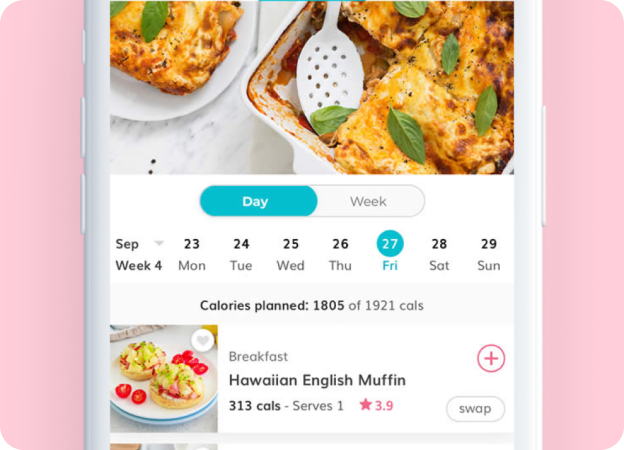
This is how many calories can be burned during sex
To burn calories (and see awesome weight loss results), sticking to a healthy meal plan and consistent exercise is key.…

10 signs you might have postnatal depression
Often we’re too busy to notice our friends might be suffering postnatal depression, but it’s important you know the…

Experts say parents should let their kids engage in more ‘risky’ play
An education expert is calling on parents to stop smothering their children and let them get their feet dirty through risky play...

25 Back To School Tricks And Tips
Over the years, this school business gets easier and you learn a few tips and tricks to make life…

Caught having sex? 11 quick witted (and hopefully believable) white lies to tell the kids
Caught with your pants down? It happens to the best of us. And it will probably happen again. So here’s…

Expecting A Baby in January or February? Here’s Some Great Names To Consider
Kicking off the New Year with a new addition? Here are some super sweet baby names designed especially for babies born in January or February.

9 Tips To Save Your Sanity When Road Tripping With Kids
Often long road trips with kids are inevitable, especially during the school holidays. One thing that isn’t compulsory is…

25 of the best family-friendly Christmas movies
To get in the holiday spirit, grab some popcorn, cozy up on the couch and watch one of these 25 family-friendly Christmas movies. Did your family's favourite make the list?

30 REMARKABLE things that will happen in your baby’s first year of life
The first 12 months after you give birth, are a crucial development period for your little one. From rolling…

12 simple lunch box hacks to save you time
We’ve pulled together 12 tried and tested lunch box hacks (from real mums like you) that will give you…

24 baby names that are inspired by HALLOWEEN!
If you’re all about pumpkins, witches and skeletons and want your baby to have a HALLOWEEN-inspired name, then check out this SPOOKY list of names!